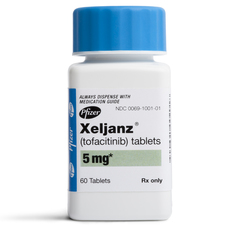
Xeljanz
The rheumatoid arthritis medication Xeljanz (tofacitinib) has been linked to several serious side effects. In fact, the drug’s label already includes a Black Box warning regarding the potential for pulmonary embolism and death among RA patients taking the twice-daily 10mg dosage regimen. In early 2021, the U.S. Food & Drug Administration (FDA) announced it was investigating a potential association between Xeljanz and an increased risk of certain cancers and heart problems.
How Does Xeljanz Work?
 Rheumatoid arthritis, also known as RA, is a progressive, chronic condition in which the body’s immune system attacks its own tissues; specifically, a thin membrane around the joints called the synovium. This results in inflammation, stiffness, and swelling in the joints. For most people, the swelling, stiffness, and joint damage associated with RA will worsen over time.
Rheumatoid arthritis, also known as RA, is a progressive, chronic condition in which the body’s immune system attacks its own tissues; specifically, a thin membrane around the joints called the synovium. This results in inflammation, stiffness, and swelling in the joints. For most people, the swelling, stiffness, and joint damage associated with RA will worsen over time.
Xeljanz is a janus kinase (JAK) inhibitor. JAKs are enzymes that work within the immune system and other cells to transmit signals that influence their function. By inhibiting JAK in immune cells, the drug interferes with the processes that cause RA.
While other RA treatments are administered via injection or infusion, Xeljanz is available in tablet form.
Tofacitinib Approval History
The FDA approved the 5 mg dose of Xeljanz in November 2012 to treat adults with moderately to severely active RA and who can’t take methotrexate.
In February 2016, Pfizer announced Xeljanz XR’s approval, an extended-release 11 mg tablets for the once-daily treatment of moderate to RA in patients who have had an inadequate response or intolerance to methotrexate.
In December 2017, the FDA approved Xeljanz to treat patients with a second condition, psoriatic arthritis, who did not respond well to methotrexate or other similar medicines called nonbiologic disease-modifying antirheumatic drugs (DMARDs)
Finally, the agency cleared the twice-daily 10mg dose of Xeljanz to treat ulcerative colitis in May 2018. However, it should be noted that the FDA has never approved this dosing regimen for the treatment of RA, and it is solely indicated for use in patients with ulcerative colitis.
Xeljanz Black Box Warning
Because it impacts the immune system, Xeljanz increases the risk that patients will develop serious, opportunistic infections, including tuberculosis. Consequently, people with an active infection should not take tofacitinib, while those who develop symptoms of an infection while using the drug should contact their doctors immediately.
A Black Box Warning on the Xeljanz label recommends that patients receive a tuberculosis test before starting treatment. The warning further notes that bacterial, fungal, viral, and other opportunistic infections leading to hospitalization and death have occurred in patients using tofacitinib. In some cases, patients have developed lymphoma and other malignancies.
Finally, the Black Box Warning suggests that kidney transplant patients taking Xeljanz along with other immunosuppressive may be vulnerable to Epstein Barr Virus-associated post-transplant lymphoproliferative disorder.
Other Xeljanz Side Effects
Other side effects potentially associated with tofacitinib include:
- Allergic reactions. Xeljanz patients should seek emergency help if they experience hives, difficulty breathing; or swelling of the face, lips, tongue, or throat.
- Severe liver symptoms. Patients should contact their doctor if they experience low fever, itching, tiredness; upper stomach pain, loss of appetite; dark urine, clay-colored stools; or jaundice (yellowing of the skin or eyes)
- Headache
- Diarrhea
- Cold symptoms such as stuffy nose, sneezing, sore throat.
Xeljanz can interact with a wide range of prescription, over-the-counter, and herbal medications. Therefore, patients should inform their doctors of any other drugs they are taking before beginning treatment with tofacitinib.
Patients should not use this medication if they suffer from severe liver disease. Additionally, they should not receive a “live” vaccination during treatment, and they should avoid contact with anyone who has.
Tofacitinib is a pregnancy category C drug. While there have been no well-controlled studies to assess its effects on pregnancy, animal studies suggest that Xeljanz may cause birth defects in a developing fetus. Therefore, it should only be used in pregnant women when the potential benefits justify the risk.
It’s unknown whether Xeljanz is excreted into breast milk. For that reason, nursing mothers should either stop taking the medication or discontinue nursing during treatment.
FDA Updates Xeljanz Black Box Warning for Pulmonary Embolism and Death
When the FDA initially approved tofacitinib, it required Pfizer to conduct a clinical trial to assess the risk of heart-related events, cancer, and opportunistic infections at two doses (10 mg twice daily and 5 mg twice daily) in combination with methotrexate. The study compared the rate of these adverse events among patients taking either Xeljanz or a tumor necrosis factor (TNF) inhibitor to treat RA. Among other things, the FDA required that RA patients enrolled in the trial be at least 50 years old and have at least one cardiovascular risk factor.
Interim results from that study have since suggested patients taking the higher dose of Xeljanz were more likely to experience a pulmonary embolism – a life-threatening blood clot that travels to the lungs — or die compared to those taking either the lower dose or a TNF blocker.
Those findings prompted the FDA to update the drug’s Black Box Warning and limit the approved use of this dosage regimen to ulcerative colitis patients who are not treated effectively or who experience severe side effects with certain other medicines. Doctors are now cautioned to prescribe the lowest effective dose possible and limit the 10mg twice-daily regimen to the shortest duration possible.
Xeljanz May Increase Risks for Cancer, Heart Problems
In February 2021, the FDA announced that the same Xeljanz study’s initial results also indicated a higher occurrence of serious heart-related events and cancer in rheumatoid arthritis patients treated with both the 5mg and 10mg doses of Xeljanz compared to patients treated with a TNF inhibitor.
“We will evaluate the clinical trial results we have received to date and will work with the drug manufacturer to obtain further information as soon as possible,” the FDA said in a communication issued on February 4th. “We will communicate our final conclusions and recommendations when we have completed our review or have more information to share.”
In the meantime, the agency is advising health care providers to consider the benefits and risks of tofacitinib when deciding whether to prescribe or continue patients on the medicine.
Patients should not stop taking Xeljanz without first consulting with their health care professionals, as doing so may worsen their condition.
- Pfizer, Inc. (October 2018) “Xeljanz Prescribing Information” http://labeling.pfizer.com/ShowLabeling.aspx?id=959
- Johns Hopkins Medicine (September 2013) “RA Pathophysiology” http://www.hopkinsarthritis.org/arthritis-info/rheumatoid-arthritis/ra-pathophysiology-2/
- Johns Hopkins Medicine (January 2013) “Tofacitinib: A novel Janus kinase inhibitor is FDA approved as the first oral biologic treatment for rheumatoid arthritis.” http://www.hopkinsarthritis.org/arthritis-news/tofacitinib-fda-approved-oral-biologic-for-rheumatoid-arthritis/
- FDA (July 2019) “Safety trial finds risk of blood clots in the lungs and death with higher dose of tofacitinib (Xeljanz, Xeljanz XR) in rheumatoid arthritis patients; FDA to investigate.” https://www.fda.gov/safety/medical-product-safety-information/xeljanz-xeljanz-xr-tofacitinib-drug-safety-communication-due-increased-risk-blood-clots-and-death
- FDA (February 2021) “Initial safety trial results find increased risk of serious heart-related problems and cancer with arthritis and ulcerative colitis medicine Xeljanz, Xeljanz XR (tofacitinib)” https://www.fda.gov/drugs/drug-safety-and-availability/initial-safety-trial-results-find-increased-risk-serious-heart-related-problems-and-cancer-arthritis
Get the latest news and litigation updates about this case by following us on Facebook. Click the "Like" button below.
Follow Us


